 |
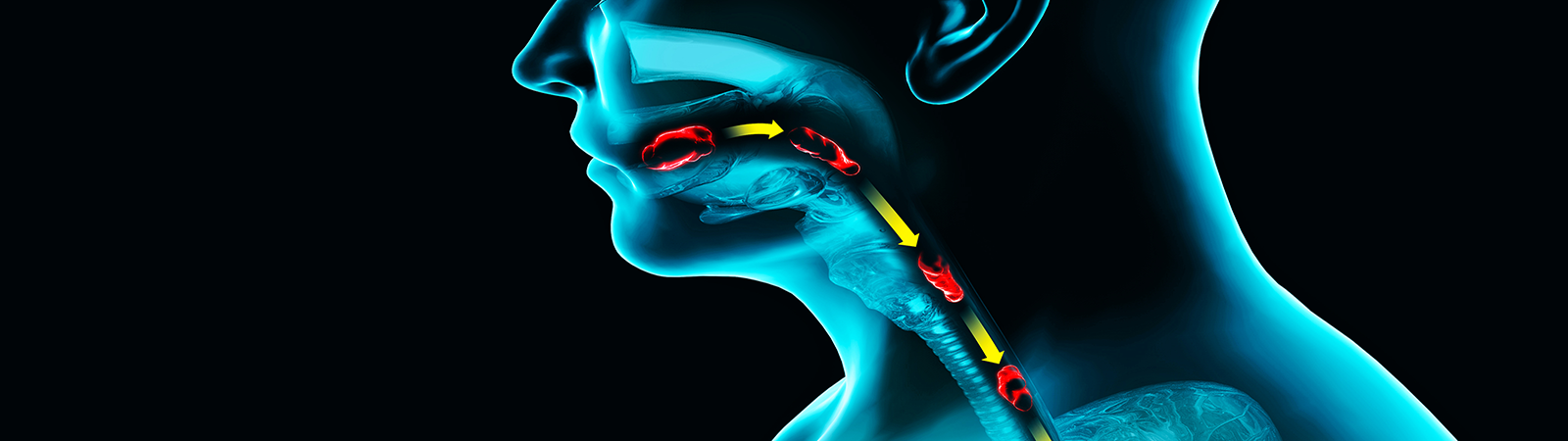
La Disfagia non è una malattia ma un sintomo, provocato dall’alterazione di una o più fasi della deglutizione, con conseguente difficoltà a far progredire il cibo e le bevande dalla bocca allo stomaco. Può causare: Esistono tre tipi di disfagia: orale, faringea ed esofagea |
 |
Disfagia Orale Disfagia faringea Disfagia esofagea |
 |
La Disfagia può portare il paziente all’isolamento sociale. Il senso di disagio che il paziente disfagico prova nel mangiare può indurlo a nascondere il problema, soprattutto nella fase iniziale. Può manifestarsi anche uno stato ansioso durante i pasti, che può indurre il paziente a rifiutare sia gli alimenti solidi che quelli liquidi. Per prevenire complicanze esistono provvedimenti adattativi (comprendono la modifica di consistenza della dieta e l’adozione di ausili speciali per l’alimentazione), manovre e posture di compenso (si corregge la postura e si modifica il processo di deglutizione) e tecniche rieducative (esercizi per facilitare o stimolare la deglutizione) |
 |
La diagnosi e la gestione della disfagia orofaringea, tipica del paziente anziano, richiedono un approccio multidisciplinare, che comprende il lavoro in equipe di infermieri, dietisti, logopedisti, nutrizionisti, neurologi, geriatri, fisiatri, gastroenterologi, otorinolaringoiatri, chirurghi, radiologi e farmacisti. |
 |
A chi assiste il malato possono essere utili i seguenti consigli: Mettere il paziente in condizione di mangiare con calma e tranquillità, in un ambiente sereno e confortevole Per ciò che riguarda la dieta, per aumentare la quota di calorie giornaliere, si consiglia di: Aumentare le porzioni o frazionare l’alimentazione in più pasti Per aumentare la quota giornaliera di proteine si consiglia di: Arricchire sughi e primi piatti cremosi con carne, pesce o affettati resi omogenei Per aumentare la quota giornaliera di liquidi si consiglia di: Utilizzare acqua gelificata (vasetti già pronti all’uso, neutri o con diversi aromi) o acqua addensata con farine istantanee Quando non si riescono a raggiungere i fabbisogni calorici proteici del paziente con la sola alimentazione modificata, si può ricorrere all’uso di supplementi nutrizionali orali cremosi o addensati, o nei casi più gravi a tecniche di nutrizione artificiale (enterale o parenterale)
|
 |
La nutrizione artificiale, spesso salvavita, è una terapia che va prescritta da medici specialisti a beneficio di pazienti portatori di patologie neurologiche o neoplastiche con alimentazione orale compromessa per un periodo di tempo superiore ai 5 giorni o in maniera permanente; in quest’ultimo caso il paziente può seguire la nutrizione artificiale anche a domicilio (NAD), sotto il controllo di un Centro specializzato e accreditato, per prevenire e trattare in maniera efficace le eventuali complicanze. Alla luce della recente legge sul testamento biologico emanata in Italia nel dicembre 2017, la nutrizione artificiale richiede il consenso informato da parte del paziente o di un suo rappresentate legale e può essere interrotta, come ogni altra terapia, quando si ravvisa il cosiddetto “accanimento terapeutico”. I familiari e i pazienti sono istruiti per la gestione della NAD e l’Unità Operativa rimane a disposizione per la verifica dell’andamento terapeutico e per eventuali cambiamenti nel corso della terapia Associazioni |
 |
Per approfondire l’argomento si consiglia Reliability and Validity of the Italian Eating Assessment Tool di Antonio Schindler, Francesco Mozzanica, Anna Monzani, Eleonora Ceriani, Murat Atac, Nikolina Jukic-Peladic, Claudia Venturini, Paolo Orlandoni. Bibliografia
|
 IRCCS INRCA
IRCCS INRCA